Category: Reconstructive Foot Surgery
In some cases, one surgery alone isn’t enough to fix a foot or ankle problem. It’s possible that the original surgeon made mistakes, or that…
Understanding Morton’s Toe
Your foot has five long bones that connect each toe to the midfoot. These bones are called…
Surgical hardware is often a part of foot surgery. There are a few different types of hardware that your foot surgeon in Sugar Land may use,…
You might be familiar with the carpal tunnel, which is the narrow passageway located at the wrist. The tarsal tunnel is a similar, narrow space,…
Bunions are bony, outward protrusions at the base of the big toe. This bump develops when the big toe bends abnormally inward, toward the other…
X-rays are an important diagnostic tool for foot doctors. They allow doctors to evaluate a problem and to track the effectiveness of the…
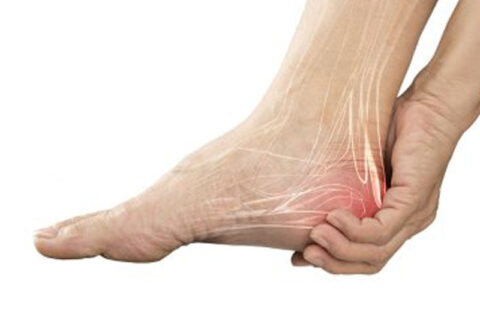
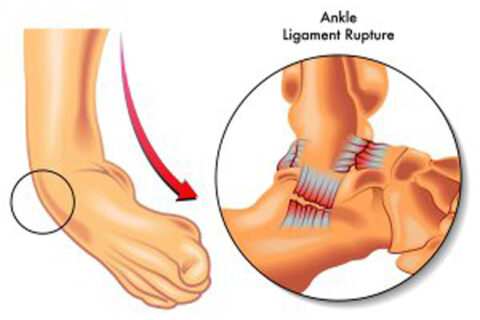
You may already know that most of the bones in your body are attached to other bones with strong, fibrous bands of tissue called ligaments. But did…
Flat feet are feet with low arches, usually caused by a muscle imbalance. This hereditary condition can cause leg pain, foot and leg fatigue,…
Foot surgeons, podiatric physicians, or foot and ankle specialists perform reconstructive foot and ankle surgeries for a number of different…
If you’ve visited a podiatrist or a foot specialist for diagnosis and treatment of a foot problem, and have since noticed that your symptoms…